AstraZeneca and Johnson Johnson vaccines are examples of adenovirus vaccines while Pfzier and Moderna use mRNA. MRNA lipids 4-hydroxybutylazanediylbishexane-61-diylbis2-hexyldecanoate 2.

How Does The Johnson Johnson Vaccine Compare To Other Coronavirus Vaccines Pbs Newshour
COVID-19 vaccines that use.

Does johnson and johnson covid 19 vaccine use mrna. It uses a different adenovirus from the one employed by Johnson Johnson. This helps the body build an immune response against the coronavirus that causes COVID-19. However Pfizer and Moderna did perform confirmation tests to ensure the vaccines work using fetal cell lines.
No the COVID-19 vaccines do not contain any aborted fetal cells. The three COVID-19 vaccines cause similar side effects including mild flu-like symptoms and injection-site reactions. The JJ vaccine also called the Johnson Johnsons Janssen COVID-19 vaccine uses an inactivated cold virus to carry genetic material which prompts your cells to create a harmless piece of the spike protein found on the surface of COVID-19.
Johnson Johnson. The most basic difference is that the Johnson Johnson vaccine is an adenovirus vector vaccine while the Moderna and Pfizer vaccines are both mRNA vaccines. The Pfizer-BioNTech and the Moderna vaccines.
Sputnik V is also an adenovirus vaccine but it is made up of two different shots. Vaccines that use this. And Johnson Johnson uses fetal cell lines in vaccine development confirmation and production.
AstraZeneca has also developed an adenovirus vaccine for COVID-19. It was produced by using cells derived from an aborted fetus in 1985. DNA is not as fragile as RNA and the adenoviruss tough protein coat helps protect the.
All of the approved COVID-19 vaccines train the body to recognize the spike protein that coats the outer surface of the coronavirus. He said its important to note that you can not get COVID-19 from the vaccine. Meanwhile the PfizerBioNTech vaccine had 95 efficacy and the Moderna vaccine had 94 efficacy at preventing symptomatic COVID-19 meaning any.
Adenovirus-based vaccines for Covid-19 are more rugged than mRNA vaccines from Pfizer and Moderna. The Pfizer-BioNTech vaccine and the Moderna vaccine are both two-dose mRNA vaccines while the Johnson Johnson vaccine is a single-shot that uses an adenovirus. A third vaccine developed by Johnson Johnson JJ Janssen uses a viral vector platform.
One week later the FDA granted EUA to another mRNA COVID-19 vaccine this one developed by Moderna. Unlike Pfizer-BioNTech vaccine and Moderna vaccine which are mRNA based vaccines the new Johnson Johnson COVID-19 vaccine is based on the development and production of adenovirus vectors. Unlike the PfizerBioNTech and Moderna vaccines which use an mRNA design the Johnson Johnson shot uses a harmless adenovirus a type of virus that typically causes the common cold.
Severe reactions to the vaccines are very rare. The code serves as an instruction manual for your immune system teaching it to recognize the virus that causes COVID-19 and attack it should it encounter the real thing. On February 27 2021 the FDA granted EUA to an adenovirus vaccine developed by Johnson Johnson.
Messenger RNA vaccines use. Also unlike the Johnson Johnson product which cannot replicate the AstraZeneca replicates in the body a limited amount. Vaccines that use this.
The COVID-19 vaccine by Johnson Johnson does not contain aborted fetus cells. There are currently three authorized COVID-19 vaccines available in the US. Both Johnson Johnson and AstraZeneca use the same vaccine technology which differs from the mRNA vaccines from Pfizer-BioNTech and Moderna.
Many people are curious to know what the ingredients are for the three currently available COVID-19 vaccines in the US. In fact the mRNA that is in the vaccine is synthetic. Two mRNA vaccines Pfizer and Moderna and one viral vector vaccine Johnson Johnson.
The full list of ingredients for the Pfizer vaccine is. Heres how the four vaccines work. This vaccine is developed by Belgian company Janssen Pharmaceuticals which is owned by Johnson Johnson.
And essentially does the same thing as the Covid-19 vaccines mentioned above. Here is a breakdown of the three COVID vaccines and their ingredients. There are two COVID-19 messenger-ribonucleic acid mRNA vaccines currently authorized for emergent use in the United States.
This adenovirus is in no way related to the coronavirus. Instead of using mRNA the Johnson Johnson vaccine uses a disabled adenovirus to deliver the instructions. Adenovirus and mRNA vaccines are the two types of COVID-19 shots currently in use.
On December 11 2020 the FDA granted emergency use authorization EUA to an mRNA COVID-19 vaccine developed by Pfizer and BioNTech.
Multisystem inflammatory syndrome -- an illness that seems to follow infection with coronavirus and impacts children -- affects multiple organs and the skin. So far a single COVID-19 patient had a rash that looked like chicken pox.
Doctors and researchers from around the world also have reported about other types of skin rashes among Covid-19 patients.

Does covid cause a face rash. Some people have reported a red itchy swollen or even painful rash where they received their COVID-19 vaccine shot. The rashes appeared on average just over 12 days from the onset of their COVID-19 symptoms. The virus triggers a number of immune reactions so it is no surprise that the skin is involved.
Other skin symptoms linked to COVID-19 have since come up. Experts say COVID-19 can cause skin rashes in all ages. The symptom has emerged in research studies of COVID-19 patients and as more is learned about the.
The side effect dubbed Covid arm has occurred in a small number of patients in the US. If your child has COVID toes you may see. This rash is extremely itchy and often starts with intense itching in the palms or soles and can cause swelling of the lips and eyelids.
The challenge with most COVID-related rashes is that it is difficult to discern whether it is COVID or some other cause says dermatologist Erum Ilyas MD. The issue is that COVID can cause a wide variety of skin signs and symptoms which is why there has been a delay in recognising that these various skin rashes were linked to the virus. Occasionally this rash develops on the fingers instead of the toes.
For many children a rash known as COVID toes may be the only sign of a coronavirus infection. Five of them developed a type of rash that looks like tiny spots called petechiae. There are other less common rashes associated with COVID-19 including Pityriasis Rosea-like light-sensitive rashes affecting the face or neck.
However according to a 2021 review the exact incidence of rash in COVID-19 remains unknown. According to the American Academy of Dermatology AAD COVID rashes can manifest as a patchy rash itchy bumps blisters that look like chickenpox round pinpoint spots on the skin a large patch with several smaller ones a lace-like pattern on the skin or lat spots and raised bumps that join together If your rash resembles any of these descriptions you should talk to your doctor. This reaction can begin from.
One of the first symptoms that COVID-19 survivors might see is a skin rash NBC News reports. According to News Medical a study published in the British Journal of Dermatology illustrates that skin rashes not only can occur as. Some general symptoms associated with many COVID-19 rashes include.
Covid-19 often triggers significant inflammation in its victims in some. It can involve any part of the body including the face. A skin rash is a possible symptom of COVID-19.
In children a coronavirus infection tends to be mild. There have also been some rare full body reactions that can look like a rash and even reports of people developing so-called COVID toes This presents as. The rash broke out into tiny blisters called vesicles.
Red or purple toes or fingers Swelling on the toes or fingers A small amount of pus. Pictured a pupuric rash which was seen on a Covid patients lower leg. A pupuric rash looks like lots of small spots of blood on the skin and is caused by blood vessels leaking 5 This.
Updated on March 16 2021. COVID-19 does sometimes have unusual dermatological symptoms of. But doctors do have a.
But they stressed that people with the harmless reaction should still get their second dose of the jab for optimal protection against Covid - around 95 per cent for the Moderna jab. 4 People reported getting rashes and feeling itchy Credit. These rashes seem to signal that the virus causes inflammation of the tiny blood vessels in the skin.
According to the National Foundation for Infectious Diseases NFID There is no influence or interaction between antibiotics and COVID-19 vaccines so when indicated antibiotics may be taken at any time relative to COVID-19 vaccine administration. But overall having allergies doesnt exclude you from getting the vaccine.
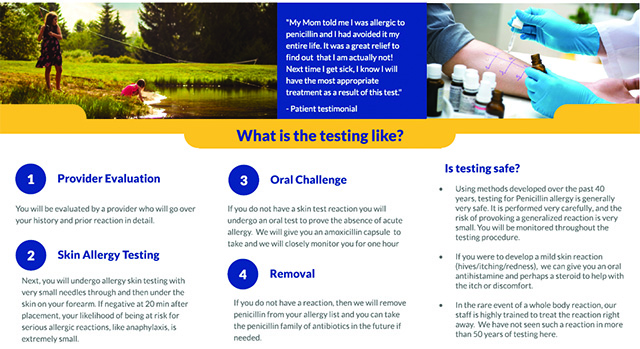
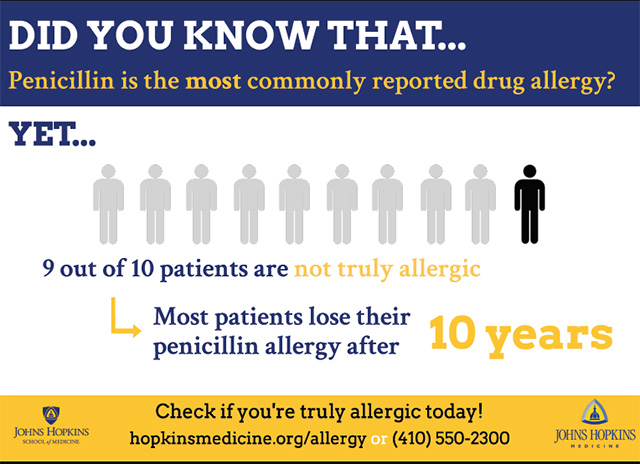
Penicillin Allergy Evaluations
Its recommended that if youve had an allergic reaction any of the ingredients in the vaccine you should not get it.
If you are allergic to antibiotics should you get the covid vaccine. However as a precaution the current recommendation is to delay vaccination if someone has any acute moderate or severe illness. Experts say those are the people who would need to be monitored for 30 minutes after receiving the COIVD-19 vaccine and may benefit from seeing. According to experts if youre allergic to polyethylene glycol you should wait to get the COVID vaccine.
Read on to find out why people with this allergy may want to hold off and for more on vaccination preparedness If You Have This Common Condition Tell Your Doctor Before the Vaccine. If you have had a severe allergic reaction or an immediate allergic reactioneven if it was not severeto any ingredient in an mRNA COVID-19 vaccine you should not get either of the currently available mRNA COVID-19 vaccines Pfizer-BioNTech and Moderna. In fact a Food Drug and Administration FDA official just confirmed that there are only two people who shouldnt get vaccine.
Previous advice from the MHRA said people with a range of allergies to food and medicines should not be given the Pfizer vaccine. The pros and cons regarding the COVID vaccine and my final decision herein. You are not at any heightened risk for a reaction to the Pfizer vaccine and you should be vaccinated.
I just had my second. Antibiotics do not affect the vaccine and it is OK to continue them. The good doctor asked if I had any history of allergic reactions to.
Per Reuters the MHRA sent out new guidance to healthcare professionals that advised Any person with a history of a significant allergic reaction to a vaccine medicine or food such as previous history of anaphylactoid reaction or those who have been advised to carry an adrenaline autoinjector should not receive the Pfizer BioNtech vaccine. Also the vaccine wont have an effect on whatever bacterial infection you are taking the antibiotics for. Last year I took my first penicillin vaccine.
If you had an allergic reaction to the first dose of a COVID-19 vaccine the CDC doesnt recommend getting the second dose. Recent research has shown that many pencillin and other antibiotic allergies identified in childhood do not persist into adulthood. Even those who have allergies to penicillin.
Dr June Raine said growing evidence from a pool of at least 800000 people in the UK and probably 15 million people in the US who have had the vaccine has raised no additional concerns. Those who have had allergic reactions to things such as food latex pollen and bee stings should still get the COVID-19 vaccine Winokur said. If you have allergies and are not comfortable with the vaccine you NEED to watch this video.
If You Are Allergic to an Ingredient in a COVID-19 Vaccine. If you have had a severe allergic reaction or an immediate allergic. The only person who has a significant contrary indication to the current mRNA vaccines are those who have allergies to.
Those who have a known allergy to one of the vaccines. These videos are based on scientific fact not speculation to g. The recommendation is contained in a fact sheet.
In other words if. Your primary care provider might recommend that you see an allergist. It is very safe for them to do that Levine said.
In the US regulators are only recommending against vaccination for people with an allergy to a specific component for PfizerBioNTech vaccine.
A very rare and unusual clotting condition. Rapid swelling of your arms or legs.

Covid Arm Some Develop Delayed Skin Reaction After Moderna Vaccine Shot Abc7 Los Angeles
Get urgent medical help if you have had an AstraZeneca vaccine in the past few days and you notice.

Allergic reaction symptoms to astrazeneca covid vaccine. Do not get the AstraZeneca vaccine if you have previously had capillary leak syndrome. These considerations include. After you have left the vaccination location seek medical attention if.
Some people will get mild short-term side effects from vaccination including injection site reactions fever joint pain muscle aches fatigue headaches or worsened eczema a day after vaccination. An immediate allergic reaction happens within 4 hours after getting vaccinated and could include symptoms such as hives swelling and wheezing respiratory distress. Additionally an allergic reaction to certain ingredients in the vaccine may occur.
Rare side effects that have been reported after AstraZeneca are. Since data and information on the systemic allergic reactions to COVID-19 vaccines are being released rapidly in current times it is our objective to review and summarize the most recent findings that exist regarding the anaphylactic reactions described for the three vaccines for COVID-19 protection and to provide an extensive description of the different excipients of the vaccines with the potential to elicit an adverse allergic reaction. O This occurs in approximately 1 in a million people getting this vaccine.
If you do have a reaction it usually happens in minutes. If You Are Allergic to an Ingredient in a COVID-19 Vaccine. These are symptoms of capillary leak syndrome.
You may also feel faint due to low blood pressure. Staff giving the vaccine are trained to deal with allergic reactions and treat them immediately. Experts refer to severe allergic reactions as anaphylaxis.
Approximately 34 of people experienced systemic side effects after the first dose of the AstraZeneca vaccine with headaches and fatigue as the leading symptom followed by chills and shivers. An adverse reaction to this jab also entails an itchy skin rash shortness of breath and swelling of the. Individuals also commonly reported pain and irritation at the site of the vaccine injection.
COVID-19 vaccination in people with allergic. Call 000 if you experience severe symptoms such as difficulty breathing wheezing a fast heartbeat or collapsing. Pain swelling tenderness redness or itching at.
If you have a serious allergic reaction to the 1st dose of a vaccine you should not have the same vaccine for your 2nd dose. Rare side effects that have been reported after COVID-19 Vaccine AstraZeneca are. Severe allergic reaction anaphylaxis.
Common side effects after COVID-19 Vaccine AstraZeneca include. You think you are having an allergic reaction. As with any vaccine you may have some side effects after receiving a COVID-19 vaccine.
The incidence of allergic reactions and deaths under investigation with the available vaccines application of vaccination in patients with mast cell disease patients who developed an allergy during the first dose vasovagal symptoms masquerading as allergic reactions the COVID-19 vaccination in pregnancy deaths associated with COVID-19 vaccination and. Severe allergic reaction anaphylaxis. The AstraZeneca Covid vaccine is used to protect people aged 18 and older against Covid.
COVID-19 vaccine side effects indicate the start of an immune response not an allergic reaction. If there is a high risk of an allergic reaction to one of the COVID-19 vaccines due to an existing allergy to PEG or Polysorbate 80 it may be possible to a have a COVID-19 vaccine that does not contain the ingredient depending on availability and with appropriate medical advice. Severe allergies should be added to the possible side effects of AstraZenecas coronavirus vaccine after likely links were found to a number of cases in Britain the EUs drug regulator said on.
O A very rare side effect of an. The five most common adverse events of Sinovacs COVID-19 vaccine are elevated blood pressure headache injection site pain dizziness and rash while the top five side effects of AstraZenecas. Serious allergic reactions to the COVID-19 vaccines are very rare.
If youve had a history of allergic. In some very rare cases symptoms can show up after 14 days with researchers estimating this happens with about one in every 100 people.

Coronavirus Incubation Period How Long Before Symptoms Appear
A prescription is needed to get this test which can be performed in authorized locations including doctors offices and emergency rooms.

How long does it take symptoms to show up for covid. Most people develop symptoms 5 to 6 days after being in contact with a person with the coronavirus. Others will develop fever with cough arriving only a few days later. A person can develop COVID-19.
From there you should wear a mask in public for 14 days until you test negative. According to the study while influenza typically begins with a cough the first symptom of COVID-19 is fever. 11 days was the median total length of stay in hospital 22 days was the time from first symptom until discharge from hospital for survivors 185 days from first symptoms until death for non-survivors 20 days median length of time for viral shedding starting at first day of symptoms.
The most common neurological symptoms appear to be cognitive changes including brain fog such as sluggishness and lack of sharpness as well as headaches sensory changes muscle or nerve pain and. But the average time before showing symptoms is thought to be 5 days. Most people who develop COVID-19 start noticing symptoms within 2 to 14 days after being exposed to the novel coronavirus known as SARS-CoV-2.
Symptoms will start to show up between two and 14 days after exposure to the virus according to Centers of Disease Control and Prevention. Symptoms of COVID-19 typically appear 214 days after exposure to the virus and the mean incubation period is 51 days. How soon after exposure to a COVID-19 case do symptoms appear.
However most people will start to experience symptoms within four or five days of exposure. This has not changed since early 2020 when the. Tests are even more accurate when patients are exhibiting symptoms.
The study found that the median incubation period was 51 days and that 975 of people with symptoms will develop these within 115 days. Its important to note that emerging research shows that people might be most likely to. This makes it portable and fast results are available within 15 minutes.
She should continue to monitor herself closely for symptoms during that time. The coronavirus incubation period which is the time between when a person is exposed to the virus and when their symptoms first appear ranges from 1 to 14 days. This news story has not been updated since the date shown.
Typical coronavirus patients develop a fever dry cough and shortness of breath but these symptoms may appear at different times or not at all. A study of 94 patients in China showed that viral load peaked shortly after the onset of symptoms indicating that people may actually be more infectious in. The incubation period for COVID-19 seems to be anywhere from three to fourteen days.
How long does it take for COVID symptoms to appear. While the incubation period for the virus can be as long as 14 days research suggests that people who are infected with SARS-CoV-2 the virus that causes the COVID-19 illness may become infectious to others several days before they start to feel ill. Evidence suggests that testing tends to be less accurate within three days of exposure and the best time to get tested is five to seven days after you were exposed.
The incubation period for COVID-19 is between 2 and 14 days. The incubation period is the length of time between when you become infected with COVID-19 and when you start to have symptoms. Fully vaccinated people should get tested for COVID-19 somewhere between three to five days after exposure.
It can take almost a week after exposure to COVID-19 to register a positive test result. Some people will start with a cough. While data on long COVID-19 has started to emerge less is known about the neurological symptoms.
However physicians working with patients with COVID-19. The puzzling nature of long COVID-19. This test is approved for use in people who are suspected of having COVID-19 and must be done within seven days of when their symptoms began.
People should consider quarantining for 14 days to stop the spread of the coronavirus. There does not appear to be any particular pattern in the order of symptom development. Among my patients exhaustion and aching all over appear to be common early signs.
The chances of having long-term symptoms does not seem to be linked to how ill you are when you first get Covid-19 and people who had mild symptoms at first can still have long. COVID-19s incubation period lasts up to 14 days. If you have the virus it.
If your sister does develop symptoms during those 14 days she will need to remain in isolation for another 10 days from the date her first symptom s appeared or until shes been without a fever for at least 24 hours whichever is longer. The CDC notes that an allergic reaction happens within four hours of getting the shot and could include symptoms such as hives swelling and wheezing. This is based on a study done in Wuhan China where the pandemic started.